What is a Chromosome?
- 2 years ago
- 0 Comments
Chromosome:
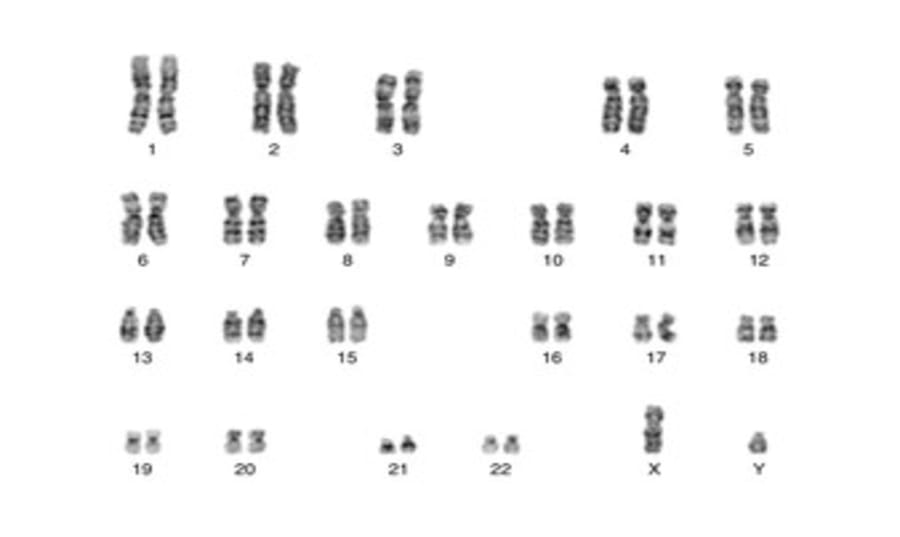
All 23 pairs of human chromosomes can be distinguished microscopically from each other, and much fine detail within each chromosome can also be recognised. An agreed international system of nomenclature, reviewed at regular intervals, forms the basis of reports from laboratories. Although these reports will usually include an explanatory text or be accompanied by an explanatory letter, clinicians may be deterred by the terminology itself, so some brief notes are given here.
Take the following example: 46,XY,t(4;22)(q32;q12)
This denotes the fact that the individual has a balanced translocation between the long arms of chromosomes 4 and 22. Several points can be noted:
- The total chromosome number is given first. In this example, there is the normal number of 46.
- The sex chromosome constitution comes next. Here the patient is chromosomally male (XY) as opposed to female (XX).
- A translocation is indicated by the letter ‘t’ with details of the chromosomes involved in brackets. In this example, chromosomes 4 and 22 are involved.
- The arms of a chromosome are indicated by the letters ‘p’ for the short arm and ‘q’ for the long arm (‘p’ is for petit, reflecting the strong French influence in early cytogenetics). In our example, the long arms of the two chromosomes are involved in the translocation. The breakpoints are given in the second brackets, indicated by numbers corresponding to band designations at points of exchange, in this case, bands q32 and q12 on chromosomes 4 and 22, respectively.
Further details in chromosome reports may deal with mosaicism (the presence of more than one cell line), inversions, ring chromosomes, the identification of particular bands on a chromosome, and the use of fluorescence in situ hybridisation (FISH) and other molecular cytogenetic techniques. If in any doubt, the clinician should make personal contact with the cytogenetics laboratory. This will provide a more meaningful idea of the problem and will allow a better assessment of risks by a discussion with cytogeneticist colleagues. Most laboratory cytogeneticists will be delighted by the opportunity to learn more specific details from the referring clinician and may in turn be able to suggest further clinical investigations from their knowledge of the phenotype associated with particular chromosomal defects.
TRISOMIES
Trisomy 21
Most cases of Down syndrome, the most important chromosome disorder, result from free trisomy of chromosome 21, and the overall population incidence (in the absence of prenatal diagnosis) is around 1 in 650 live births. It may have increased in recent years in countries where women have delayed pregnancy to a later age. Early and rapid chromosome analysis is important in all clinically suspected cases since the clinical diagnosis, though usually clear, is not always so and the risk of potential complications is considerable.
It is important to note the following points:
● The incidence in offspring of young women (25 years and under) is very low at 1 in 1,000. It may rise again slightly in the youngest mothers.
● The chance does not rise above that of the overall population incidence until a maternal age of around 30 years.
● The chance of a Down syndrome child reaches 1% at a maternal age of about 40 years and rises steeply thereafter, with a slight fall possible in the few births to women in their late 40s. Increasing use of in vitro fertilisation (IVF) procedures in older women point to the need for more accurate data for this group.
Other viable autosomal trisomies (13, 18 and 22)
Other trisomies are rare (as live births) in comparison with trisomy 21. Recurrence is uncommon except for translocation cases but data are few; most age-related recurrence risks will be for the more common Down syndrome, for which the risks given earlier should be used. Maternal age is also a factor; it gives the age-specific risks for trisomies 18 and 13 at amniocentesis. The live-birth risks are considerably lower because of the frequency of spontaneous abortion, being around one-third the rate at amniocentesis for trisomy 18 and one-sixth that for trisomy 13. Since trisomy 13 can be due to a translocation (either Robertsonian or reciprocal), and both conditions may also be mimicked by non-chromosomal (often autosomal recessive) disorders, cytogenetic analysis (a karyotype) is essential in any suspected case.
Non-viable autosomal trisomies (e.g. trisomy 16) are extremely common in spontaneous miscarriages, and it is questionable whether amniocentesis in a subsequent pregnancy is warranted when such an abnormality is detected; non-invasive prenatal testing (NIPT) has altered practice in this area. How far risks for a future live-born child are increased by a previous chromosomally abnormal miscarriage or stillbirth is still uncertain; if the abnormality was a late miscarriage or stillbirth, then it seems prudent to use the same risk figures as for a live birth until better figures are available.
In triploidy, there is a complete additional set of chromosomes. It is frequent as a cause of spontaneous pregnancy loss but is usually sporadic. Live birth is exceptional. There are phenotypic differences between the two different types of triploidy, in the fetus and the placenta, depending upon whether there is a 2:1 or 1:2 ratio of paternally derived to maternally derived chromosomes, with the molar changes of a partial hydatidiform mole indicating that the paternally derived chromosomes are present in excess.
SEX CHROMOSOME ABNORMALITIES
Recurrence in a family is exceptional for any of the sex chromosome abnormalities. Even among the offspring of affected fertile individuals, transmission is rare, for reasons not fully understood. The 45, X (Turner) syndrome is very common at conception, but most cases miscarry spontaneously. It is frequently associated with aortic coarctation and almost invariably with streak gonads, primary amenorrhoea and short stature. Despite the apparent mildness of phenotype in most children with Turner syndrome, a wide range of clinical problems may occur in later life, most notably cardiovascular disease. Mosaic patients or those with partial deletions of the X chromosome may show streak gonads without the full phenotypic features, as may isochromosomes. During pregnancy, oedema may be reflected in abnormal nuchal thickness on prenatal ultrasound testing.
CHROMOSOME TRANSLOCATIONS
Translocation Down syndrome 
The great majority of cases of Down syndrome have 47 chromosomes owing to trisomy 21, but in about 5% of cases the chromosome number is normal (i.e. 46) and the extra chromosomal material is translocated onto another chromosome. This type of rearrangement is known as a Robertsonian translocation. Most commonly, the second chromosome is involved in chromosome 14, and less commonly chromosome 22, 13, 15 or even another chromosome 21.
INVERSIONS
The rearrangement of genetic material within a chromosome is usually recognised by chromosome banding techniques but is also revealed by whole-genome sequencing. When the rearrangement is confined to one arm of a chromosome (paracentric inversion), the risk of abnormality in the offspring is small (3% has been suggested). However, if the centromere is involved (pericentric inversion) in an autosome, this may cause problems in pairing with the homologous chromosome at meiosis, so that gametes with an unbalanced chromosome complement may be formed. This may be discovered in a parent after a child with an unbalanced chromosome abnormality has been born, or it may be an incidental finding.
MOSAICISM
A chromosomal mosaic is an individual whose organs contain more than one chromosomally distinct line of cells. When one of the cell lines is normal (e.g. 45, X/46, XX Turner mosaicism), the phenotype of the individual will usually be intermediate between the full disorder and normal. Some chromosome disorders are only known in mosaic form (e.g. mosaic trisomy 8, and mosaic 12p tetrasomy or Pallister-Killian syndrome), the full condition probably being lethal.
DELETIONS
Deletions involve visible loss of a part of a chromosome (under the microscope). Phenotypic features are less severe than when an entire chromosome is lost, so they are seen involving chromosomes where complete loss is incompatible with a full-term pregnancy. Some of the increasing numbers of abnormalities give relatively specific clinical features.
MICRODELETION SYNDROMES
Several techniques can now be used to identify small chromosomal deletions that would usually not be identified when performing a standard karyotype. These include sophisticated banding techniques, often carried out early in mitosis when the chromosomes are in a relatively elongated phase. Microdeletions can also be readily detected through the use of FISH or multiplex ligation-dependent probe amplification (MLPA) (if a specific microdeletion is suspected) or with array CGH.



Leave Comment